
PROMO!
First order? Get 10% OFF with this code: 1storder
Written by

Menopause brings hormonal changes that affect millions of women worldwide. Researchers study HMG derived from postmenopausal urine in reproductive endocrinology and fertility research.
Human Menopausal Gonadotropin (HMG) contains both follicle-stimulating hormone and luteinizing hormone. These hormones work together to support reproductive research, especially in ovulation induction and controlled ovarian stimulation studies.
Scientists study HMG, which contains glycoprotein hormones, mainly in fertility-focused research. Current research looks at HMG treatment protocols in reproductive endocrinology rather than menopause symptom management.
At Peptide Works, we provide research-grade peptides for scientific studies only. These compounds support laboratory research and are not intended for human consumption.
Discover HMG Peptide from Peptide Works, a targeted peptide designed to support hormonal balance and help manage menopausal symptoms naturally.

Menopause triggers big shifts in estrogen and progesterone production within women’s bodies. Research shows these dropping hormone levels create changes throughout many body systems.
Scientists studying HMG treatment observe how gonadotropin levels change during this time. Lab studies reveal that luteinizing hormone increases 3-fold and follicle-stimulating hormone becomes much higher during menopause.
| Hormone/Chemical | Pre-Menopause | Post-Menopause | Primary Effects |
|---|---|---|---|
| Estrogen | Normal levels | Significant decrease | Hot flashes, mood changes, bone loss |
| Progesterone | Cyclical production | Minimal levels | Sleep problems, anxiety |
| Serotonin | Stable production | Notable decline | Depression, sleep issues |
| Dopamine | Regular activity | Significant decline | Low motivation, reduced pleasure |
| FSH/LH | Low-moderate | FSH: 10-20x, LH: 3x increase | Hormone surges, physical symptoms |
These hormone changes contribute to hot flashes, mood swings, and sleep problems. Understanding these changes helps researchers develop targeted approaches using peptides like HMG for scientific study. This research helps scientists see how reproductive hormones connect to mental health during menopause.
Hot flashes affect over 80% of women going through menopause. These sudden heat surges happen when dropping estrogen levels confuse the brain’s temperature control center.
Research shows that HMG treatment may help stabilize hormone receptor activity in lab studies. Mood swings occur because hormone changes affect brain chemicals like serotonin and dopamine.
During menopause, serotonin levels can drop substantially because estrogen helps make this mood chemical. Dopamine, which affects motivation and pleasure, also goes down as hormone levels fall.
These changes in brain chemicals often cause feelings of depression, anxiety, and irritability. Scientists observe that luteinizing hormone spikes can trigger both physical and emotional symptoms together.
Studies indicate that combined HMG and Sermorelin peptide research may address multiple pathways. These findings help researchers understand how peptides might support hormonal balance during menopause.
Menopause often causes depression, anxiety, and irritability in many women. These emotional symptoms happen due to shifts in hormone levels, especially dropping estrogen.
Studies show these mood changes impact daily life and overall well-being. Scientists studying menopause research how changes in estrogen affect serotonin and dopamine, two brain chemicals involved in mood regulation.
Researchers focus on how fluctuating hormone levels influence these brain chemicals. Studies suggest that keeping hormone levels steadier through standard menopausal hormone therapy may help improve mood in some women.
While research continues into how hormones affect mental health during menopause, there is currently no strong clinical evidence that HMG treatment or peptide therapy directly regulates serotonin or dopamine or treats menopause-related mood symptoms. This ongoing research helps develop better, evidence-based ways to support women facing hormonal changes.

Menopause often causes depression, anxiety, and irritability in many women. These emotional symptoms happen due to shifts in hormone levels, especially dropping estrogen.
Studies show these mood changes impact daily life and overall well-being. Scientists studying HMG treatment research how peptide therapy might improve mental health during menopause.
Researchers studying HMG treatment look at how gonadotropins affect these brain chemicals in labs. Studies suggest that keeping hormone levels steady could help balance mood better.
Peptide therapy may play a role in controlling these mood-related chemicals. This research helps develop better ways to support women facing hormonal changes.
Peptide therapy is a growing focus in menopause research today. Scientists study how HMG treatment and Sermorelin may improve hormonal balance. These peptides support natural hormone production and receptor activity in laboratory studies.
Combined protocols show promise in addressing multiple menopausal symptoms together. Research indicates HMG treatment might regulate mood, energy levels, and bone health indirectly.
Sermorelin peptides stimulate the pituitary gland to release human growth hormone. This hormone helps regulate metabolism, energy, and tissue repair.
During menopause, sermorelin can support hormonal balance naturally. It encourages the body to release growth hormone in natural pulses.
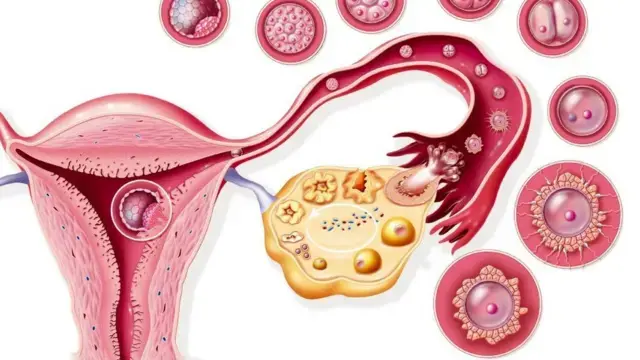
HMG (human menopausal gonadotropin) supplies follicle-stimulating and luteinizing hormone activity to stimulate ovarian follicles. Clinical research on ovarian stimulation, such as IVF and ovulation induction, shows that this increases estradiol in women with responsive follicles. It is widely used for ovulation induction and assisted reproduction.
In established menopause, ovarian function is minimal or absent due to follicle depletion. Given this, HMG cannot reliably raise estrogen levels or relieve common symptoms such as hot flashes, night sweats, mood swings, or vaginal dryness. Its mechanism requires a follicular response, which is lacking.
Research evaluating HMG focuses on fertility outcomes, not menopausal symptom management. Evidence from clinical trials supports symptom relief via estrogen-based hormone therapy or other non-hormonal treatments that target vasomotor and genitourinary symptoms.
Sermorelin binds growth hormone-releasing hormone receptors on pituitary somatotroph cells. Sermorelin mimics natural GHRH and triggers growth hormone secretion through cAMP signaling and adenylyl cyclase activation. Sermorelin maintains pulsatile GH release under somatostatin control.
Sermorelin raises plasma GH levels to treat growth hormone deficiency. Sermorelin improves energy, sleep, and body composition in these cases. These effects align with some hormonal shifts seen in menopause.
Explore Sermorelin from Peptide Works, a peptide studied for its potential to support natural growth hormone release and overall vitality.
The future of HMG treatment research looks promising as scientists explore new ways HMG works. Research will focus on how HMG interacts with other peptides like Sermorelin.
Researchers plan to study how HMG treatment affects genes and cellular signaling in greater detail. Advanced lab techniques will help uncover new HMG applications in menopausal hormone regulation.
Current investigations continue to reveal promising applications for women experiencing menopausal transitions. These scientific advances offer hope for more effective and safer treatment options in the coming years.
All research remains focused solely on laboratory settings, with Peptide Works continuing to supply research-grade HMG and related peptides for these vital scientific studies worldwide.
All peptides and compounds mentioned are strictly for research purposes only and not for human use.
[1] Gleicher N, Karande V. Generic human menopausal gonadotropin (hMG) in place of more costly follicle-stimulating hormone (FSH) for routine ovulation induction. J Assist Reprod Genet. 2000 Oct;17(9):489-95.
[2] Ginsburg J, Hardiman P. Ovulation induction with human menopausal gonadotropins–a changing scene. Gynecol Endocrinol. 1991 Mar;5(1):57-78.
[3] Walker RF. Sermorelin: a better approach to management of adult-onset growth hormone insufficiency? Clin Interv Aging. 2006;1(4):307-8.
[4] Shi S, Hong T, Jiang F, Zhuang Y, Chen L, Huang X. Letrozole and human menopausal gonadotropin for ovulation induction in clomiphene resistance polycystic ovary syndrome patients: A randomized controlled study. Medicine (Baltimore). 2020 Jan;99(4):e18383.
ALL CONTENT AND PRODUCT INFORMATION AVAILABLE ON THIS WEBSITE IS FOR EDUCATIONAL PURPOSES ONLY.
DISCLAIMER: These products are intended solely as a research chemical only. This classification allows for their use only for research development and laboratory studies. The information available on our Peptide Works website: https://peptide-works.com/ is provided for educational purposes only. These products are not for human or animal use or consumption in any manner. Handling of these products should be limited to suitably qualified professionals. They are not to be classified as a drug, food, cosmetic, or medicinal product and must not be mislabelled or used as such.
Peptide Works
Related Articles
Can Growth Hormone Peptides Cause Cancer?
Current research examines whether growth hormone peptides present cancer risks in laboratory studies. Recent studies focus on synthetic substances like

Is Tesofensine an Appetite Control Capsule?
Tesofensine is a research compound studied for its impact on weight management and appetite control. Unlike standard appetite control capsules,

Best Peptides for Women in Perimenopause: From Libido to Energy
Do you feel drained, struggle with focus, or notice your drive slipping during perimenopause? These common symptoms can feel frustrating.