PROMO!
First order? Get 10% OFF with this code: 1storder
Written by
KPV is a lysine-proline-valine tripeptide studied as an anti-inflammatory peptide because it restrains NF-κB activity, lowering TNF-α and IL-6 in gut and skin models. BPC-157 has been shown in preclinical studies to modulate cytokine surges and protect endothelial junctions, helping reduce edema after chemical colitis. TB-500, a thymosin β-4 fragment, binds actin, accelerates cell migration, and promotes angiogenesis in muscle injury assays.
Early rodent and cell-culture studies report consistent anti-edema and healing effects. Together, these three peptides allow researchers to map injury-repair signals without the broad reach of traditional immunosuppressants. Peptide Works supplies KPV, BPC-157, and TB-500 worldwide for research use only, supporting controlled studies on anti-inflammatory peptide pathways.
While KPV shows anti-inflammatory properties across multiple tissue types, its exact mechanisms in gastrointestinal inflammation deserve closer examination.
Explore KPV from Peptide Works, an anti-inflammatory peptide that calms gut inflammation by lowering NF-κB activity and supporting intestinal healing.

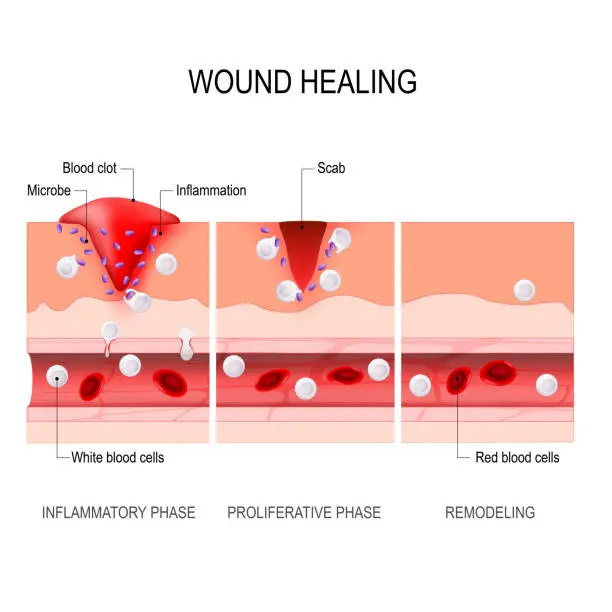
KPV enters intestinal epithelial cells through the PepT1 transporter and lowers NF-κB activation. This reduces TNF-α, IL-6, and other cytokines in colitis models. The result is smaller ulcers, improved barrier healing, and less edema.
Some studies suggest KPV also helps preserve tight-junction proteins, though timing varies across experiments. As a precision anti-inflammatory peptide, it targets gut inflammation without broad immunosuppression.
Researchers often pair KPV with BPC-157 for barrier support or TB-500 for actin-driven tissue repair. This pairing creates multi-angle mapping of IBD and leaky-gut pathways. These data place KPV at the center of intestinal-healing peptide studies. Future trials may reveal dosage ranges that maximize recovery while limiting off-target effects.
Understanding KPV’s gut-specific actions provides context for how BPC-157 reduces inflammation through different cellular pathways.
BPC-157 is a 15-amino-acid “body-protection” peptide that quiets inflammation on multiple fronts. It reduces TNF-α, IL-1β, and IL-6 by damping nitric-oxide and NF-κB loops that drive cytokine bursts. It also supports gut– and vessel-lining junctions, limiting plasma leaks that fuel tissue edema.
In addition, BPC-157 promotes angiogenesis and collagen formation, with effects linked to VEGF-related pathways in some models. These combined actions make BPC-157 a complementary anti-inflammatory peptide next to KPV’s NF-κB brake and TB-500’s actin-guided migration useful for side-by-side pathway studies.
BPC-157’s broad tissue protection contrasts with TB-500’s more focused role in cell repair and migration.
Discover BPC-157 from Peptide Works, a protective peptide that reinforces gut lining, aids angiogenesis, and reduces tissue inflammation.
TB-500, a thymosin β-4 fragment, binds G-actin and frees cells to migrate into injured muscle and tendon. That actin shift sparks angiogenesis: VEGF rises, new capillaries form, and oxygen reaches the wound. A single rat limb-injury study reported lower prostaglandin E2 after TB-500 treatment; broader confirmation is still pending.
Rodent limb-injury studies report faster recovery when TB-500 follows KPV’s NF-κB brake or BPC-157’s barrier support. These complementary actions let scientists stack peptides, trace regeneration loops, and test dosing without overlap keeping each anti-inflammatory peptide in its own mechanistic lane.
The distinct pathways of these three peptides create opportunities for tackling complex inflammatory conditions such as intestinal permeability.
Checkout TB-500 from Peptide Works, an anti-inflammatory peptide fragment that binds actin to boost cell migration, angiogenesis, and muscle repair.
KPV lowers NF-κB activation, reducing TNF-α and IL-6 that loosen junctions in DSS colitis mice. BPC-157 boosts tight-junction proteins like claudin-1 and occludin, restoring barrier strength and mucosal thickness in similar models.
TB-500 adds angiogenic support; its thymosin β-4 core lifts VEGF, helping new epithelium form. Since each peptide addresses a different “leak trigger” signal brake, junction seal, vascular support researchers now explore stacked protocols to normalize zonulin and LPS in experimental systems without broad immunosuppression.
Beyond local tissue repair, these peptides may also support control of systemic inflammation that strains normal immune balance.
KPV reduces NF-κB activation, blunting TNF-α and IL-6 surges. BPC-157 steadies inflammatory loops and promotes repair. TB-500 enhances cell migration and angiogenesis, supporting cleanup while limiting lingering inflammation.
Preclinical studies in sepsis and hyper-inflammation models suggest peptides may help reduce cytokine peaks and shield organs without full immune shutdown. The extent of these effects, especially in combinations, is still being tested. These early findings have led to new trials of peptide strategies for cytokine control in lung and gut models.
With each peptide hitting different checkpoints, comparisons reveal unique strengths in lab studies.
KPV, BPC-157, and TB-500 each target a different point in the inflammatory cascade. The “best” peptide depends on the study endpoint rather than a single winner.
| Peptide | Main Molecular Target | Primary Research Benefit | Typical Models |
|---|---|---|---|
| KPV | Lowers NF-κB activity | Sharp TNF-α / IL-6 drop in colitis models | Colitis, dermatitis |
| BPC-157 | Supports junctions, aids angiogenesis | Restores barrier integrity, tissue repair | “Leaky gut”, tendon |
| TB-500 | Binds G-actin, drives migration | Speeds muscle-tendon repair, supports angiogenesis | Muscle, ligament |
Combining peptides lets researchers study cytokines, barrier function, and tissue remodeling together without pathway overlap. All three compounds are offered by Peptide Works strictly for laboratory investigation.
As research continues, these approaches may open the way to broader clinical applications.
Research shows that peptides like KPV, BPC-157, and TB-500 may work best in combination. KPV brakes inflammation signals. BPC-157 supports barrier repair and angiogenesis. TB-500 helps cells migrate and heal. Pre-clinical teams have begun designing pilot studies that combine two or three peptides, but peer-reviewed results are not yet available.
As more studies confirm safety and efficacy, these peptides could guide new strategies for managing inflammation and supporting tissue recovery.
Peptide Works supplies these compounds worldwide, supporting research that may change how we approach inflammation and tissue repair.
All products discussed are supplied for research purposes only and are not intended for human use.
[1] Dalmasso G, Charrier-Hisamuddin L, Nguyen HT, Yan Y, et al. PepT1-mediated tripeptide KPV uptake reduces intestinal inflammation. Gastroenterology. 2008 Jan;134(1):166-78.
[2] Kannengiesser K, Maaser C, Heidemann J, Luegering A,et al. Melanocortin-derived tripeptide KPV has anti-inflammatory potential in murine models of inflammatory bowel disease. Inflamm Bowel Dis. 2008 Mar;14(3):324-31.
[3] Keremi B, Lohinai Z, Komora P, Duhaj S, et al. Antiinflammatory effect of BPC 157 on experimental periodontitis in rats. J Physiol Pharmacol. 2009 Dec;60 Suppl 7:115-22.
[4] Samaddar A, Kakkar A, Sakthivel P, Kumar R, et al. Cytological diagnosis of solitary fibrous tumour of the lacrimal sac: Role of immunocytochemistry for STAT6. Cytopathology. 2021 Jan;32(1):115-119.
[5] Reich SH, Melnick M, Davies JF 2nd, Appelt K, et al. Protein structure-based design of potent orally bioavailable, nonpeptide inhibitors of human immunodeficiency virus protease. Proc Natl Acad Sci U S A. 1995 Apr 11;92(8):3298-302.
ALL CONTENT AND PRODUCT INFORMATION AVAILABLE ON THIS WEBSITE IS FOR EDUCATIONAL PURPOSES ONLY.
DISCLAIMER: These products are intended solely as a research chemical only. This classification allows for their use only for research development and laboratory studies. The information available on our Peptide Works website: https://peptide-works.com/ is provided for educational purposes only. These products are not for human or animal use or consumption in any manner. Handling of these products should be limited to suitably qualified professionals. They are not to be classified as a drug, food, cosmetic, or medicinal product and must not be mislabelled or used as such.
Peptide Works
Related Articles

What are the Best Cognitive Peptides?
Cognitive peptides are short chains of amino acids that researchers are exploring for their potential effects on brain function. They

Achieving increased skin pigmentation without prolonged sun exposure has been demonstrated with Melanotan peptides in research. Two commonly studied options,

Can PTD-DBM Hair Growth Peptide Stop Balding?
Hair thinning and balding affect millions worldwide, often leading to frustration and limited options. This challenge has driven researchers to