Fertility peptides are receiving growing attention in research. Researchers study peptides like Gonadorelin, HCG, and PT-141 for their potential to support reproductive health and hormone balance.
These peptides are intended strictly for research and not for human use. Early studies suggest fertility peptides may help improve how the body’s reproductive system functions.
At Peptide Works, we provide these peptides to researchers worldwide, supporting the advancement of fertility research through reliable peptide supply.
Understanding the role these peptides play in regulating hormones offers deeper insight into their broader effects on reproductive health.
Explore Gonadorelin from Peptide Works, a peptide that stimulates natural hormone release to support reproductive hormone cycles.
How Do Fertility Peptides Support Hormone Balance?

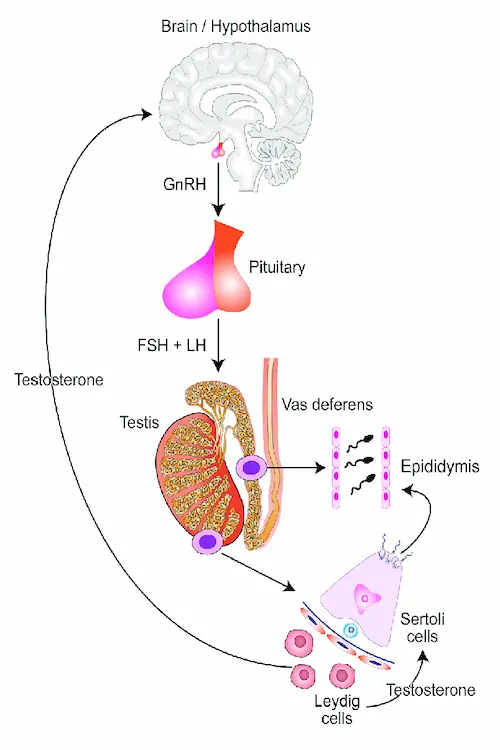
Fertility peptides, made up of specific sequences of amino acids, help control the body’s natural hormone systems. Gonadorelin tells the brain to release GnRH, which then triggers LH and FSH hormones. These hormones guide ovulation in women and testosterone in men.
HCG fertility treatment helps develop ovarian follicles and improve embryo quality. PT-141 acts on melanocortin receptors in the brain especially MC4R to influence sexual arousal and brain signals tied to hormone-related behavior.
Recent studies continue to explore how these amino acid-based peptides interact with hormone pathways, offering deeper insight into their roles in reproductive health and hormone regulation. Researchers study these peptides to understand hormone control and reproductive health.
While the hormonal systems they influence are shared, the ways fertility peptides function in men and women are often quite different.
Discover HCG from Peptide Works, a peptide that mimics LH to support testosterone levels, ovarian follicle development, and fertility function.
How Do Fertility Peptides Work Differently for Men and Women?
Fertility peptides affect men and women in different ways by controlling separate hormone processes. In men, Gonadorelin signals the brain to release GnRH. This boosts LH and FSH, which raise testosterone and improve sperm quality. These peptides also help keep hormones balanced, which may support prostate function and overall reproductive health.
HCG can raise sperm production and keep the testicles healthy when other hormones are used. PT-141 acts on brain pathways to increase sexual desire and may improve mood and performance. However, there is no clear proof that PT-141 directly improves sperm quality or fertility in men.
In women, Gonadorelin and HCG support ovulation rate and help granulosa cells feed developing eggs inside the female reproductive tract for better growth and maturation. This strengthens the reproductive process. Obesity and other risk factors can change peptide and hormone signals, which may affect how these peptides influence fertility.
PT-141 is sometimes used to increase low desire and has been studied for treating sexual dysfunction, including erectile dysfunction in men. These peptides allow fertility support to be matched to the specific needs of men and women.
This difference in hormone responses leads to a closer look at male fertility, especially sperm quality and hormone balance.
How Do Fertility Peptides Affect Sperm Quality and Male Hormone Cycles?

Fertility peptides help enhance sperm health by supporting hormone balance in the testes over time. Gonadorelin encourages steady hormone release that promotes healthy sperm development and maturation.
HCG activates Leydig cells to maintain testosterone levels key for sperm motility and vitality. Balanced hormone levels may also help reduce oxidative stress, which damages sperm membranes and DNA. Studies using a control group have shown that HCG significantly improves sperm parameters in men with low testosterone. These peptides also aid in stabilizing hormone fluctuations that impact sperm production.
PT-141’s influence on brain pathways can improve sexual function, which may offer indirect benefits to male fertility. However, direct improvements in sperm quality from PT-141 remain unproven.
Reported side effects of PT‑141 include nausea, flushing, headache, temporary blood pressure changes, and injection site reactions.
To fully appreciate how these hormonal signals translate into fertility benefits, it helps to understand the role of Leydig cells.
Checkout PT-141 from Peptide Works, a peptide that activates brain receptors to enhance sexual desire and influence hormone-related behavior.
How Do Leydig Cells Affect Male Fertility?
Leydig cells are key for male fertility because they make testosterone in the testes when activated by LH, a pituitary hormone.
Consistent testosterone from Leydig cells is vital for healthy sperm production, supporting sperm growth and motility for natural conception.
Factors like LH, HCG, and some fertility peptides can stimulate these cells to keep testosterone at needed levels in the body.
Poor Leydig cell function lowers testosterone, leading to weaker sperm and male infertility. Supporting Leydig cells can help boost natural sperm quality and maintain strong fertility in men.
Of course, testosterone itself plays a major role in fertility especially when it comes to sperm motility and function.
How Does Testosterone Influence Sperm Motility and Male Fertility?
Testosterone is needed to produce healthy and active sperm in men. Good levels help sperm grow, keep their shape, and move well, which is important for natural fertilization.
If testosterone drops too low, sperm may move slower and look abnormal, which can lower fertility and make pregnancy harder.
Natural hormones like LH and some fertility peptides help keep testosterone at the right level. But extra testosterone from medicines or supplements can reduce sperm and harm motility.
Keeping testosterone balanced helps sperm move well and supports fertility, especially with proper hormone care.
While natural conception is one path, researchers are also looking at how these peptides may play a role in assisted reproductive technologies like IVF.
Can Fertility Peptides Improve IVF Success Rates?
Fertility peptides such as GnRH agonists and HCG are used only for laboratory research. This includes in vitro (lab-based) and in vivo (living organism) studies linked to in vitro fertilization (IVF). They are not for personal or clinical use.
Studies in research show these peptides may help ovaries make more eggs and support balanced hormone signals for IVF cycles.
Some peptides, such as research-grade growth hormone, are also being investigated for their potential to improve egg quality and embryo development. However, these remain strictly experimental and are not part of approved IVF protocols.
Benefits appear most for certain IVF challenges in scientific studies. Findings are still early, and use is limited to controlled research environments.
The potential these peptides show in labs today hints at what’s possible tomorrow.
The Future of Fertility Peptides
Fertility peptides are showing promise in research, with new studies exploring how they support hormone balance, egg and sperm quality, and IVF outcomes.
As science advances, more labs are testing these peptides for conditions like polycystic ovary syndrome (PCOS) and other hormone-related fertility challenges, aiming to find safer and more effective ways to help fertility issues.
Peptide Works is proud to be an online retailer, supplying researchers in the United States and worldwide with top-quality fertility peptides for scientific discovery. While these products are not for human use, they play a key role in advancing research and supporting the search for future fertility solutions.
All products discussed are supplied for research purposes only and are not intended for human use.
References
[1] Leão IMR, Consentini CEC, El Azzi MS, Anta-Galván E, et al. Effect of gonadorelin dose and an additional gonadorelin treatment 2 days after the initiation of Resynch-25 on ovarian dynamics and fertility of lactating Holstein cows. J Dairy Sci. 2025 Mar;108(3):2914-2932.
[2] Alyasin A, Mehdinejadiani S, Ghasemi M. GnRH agonist trigger versus hCG trigger in GnRH antagonist in IVF/ICSI cycles: A review article. Int J Reprod Biomed. 2016 Sep;14(9):557-566.
[3] Lee JA, Ramasamy R. Indications for the use of human chorionic gonadotropic hormone for the management of infertility in hypogonadal men. Transl Androl Urol. 2018 Jul;7(Suppl 3):S348-S352.
[4] Babak J, Behruz F, Mohammadreza Y, Morteza FK. The Effect of Human Chorionic Gonadotropin Therapy on Semen Parameters and Pregnancy Rate after Varicocelectomy. Curr Urol. 2018 Feb;11(2):92-96.
[5] Edinoff AN, Sanders NM, Lewis KB, Apgar TL, et al. Bremelanotide for Treatment of Female Hypoactive Sexual Desire. Neurol Int. 2022 Jan 4;14(1):75-88.