PROMO!
First order? Get 10% OFF with this code: 1storder
Written by

HMG hormone has both FSH and LH activity. It is studied for stimulating ovarian follicles and helping oocyte growth in fertility research. Researchers compare HMG with recombinant FSH. Some results suggest benefits for hormone balance and steady follicle development in controlled experiments.
hCG is often used after HMG. It can complete maturation and prepare oocytes for collection in assisted reproduction studies. Studies note follicle size, egg quality, and hormone levels to measure effects.
At Peptide Works, we sell high-quality research peptides, including HMG, for research purposes only, not for human or veterinary use. Because HMG is often followed by a final maturation step, it’s useful to look at how hCG acts in this role.
Discover HMG Peptide from Peptide Works, supporting ovarian stimulation and follicle growth in advanced fertility treatment studies.
After HMG hormone use, HCG fertility treatment works like an LH signal, telling the eggs to finish maturing before planned retrieval procedures. Research often sets egg retrieval around 36 hours after hCG so eggs reach peak maturity with better quality and fertilization chances.
This LH-like effect completes egg cell division, supports cell expansion around the egg, and prepares them for safe handling during procedures. Studies show the exact timing of hCG after HMG can change embryo quality, fertilization rates, and later results in reproduction research.
Since timing is critical to success, researchers have studied the optimal timeframe for retrieval after an hCG trigger.
Explore hCG Peptide from Peptide Works, aiding final oocyte maturation and timing in fertility research protocols.
After HMG hormone use, many programs plan egg retrieval about 36 hours after hCG to match peak maturation and prevent premature ovulation. Studies show effective timing can range from 32 to 38 hours, with some research supporting 36 to 39 hours for mature oocyte collection.
| Protocol / Trigger Type | Typical Retrieval Window (hours) | Key Research Notes |
|---|---|---|
| Standard hCG trigger | ~36 | Matches peak oocyte maturation; helps avoid premature ovulation |
| Recombinant hCG trigger | 36–39 | Some studies find ~37h may improve pregnancy rates in specific protocols |
| General clinic practice | 32–38 | Adjusted according to follicle monitoring and individual ovarian response |
Cohort studies suggest aiming for 37 hours may improve pregnancy rates in certain protocols using recombinant hCG triggers for stimulation. Earlier trials found more mature eggs and better embryo quality when retrieval occurred at or beyond 36 hours compared with shorter intervals.
These findings led to closer comparisons of different trigger‑to‑retrieval intervals to see how they affect embryo development.
Studies show longer gaps between hCG trigger and egg retrieval can produce embryos with better shape, fewer fragments, and steadier development. Lab findings suggest extra time may improve egg cell readiness, helping early division and blastocyst growth happen in a balanced, healthy way.
In HMG hormone cycles, some clinics report more top-quality embryos when timing is adjusted for each patient’s follicle growth and hormone profile.
Reviews note timing choice can affect implantation chances, leading experts to explore customized schedules based on each woman’s ovarian response patterns.
Once embryos are formed, attention often turns to whether their quality can indicate implantation potential.
Yes. Higher embryo quality is linked with better implantation odds, including when using single euploid transfers in controlled protocols. Among euploid blastocysts, stronger inner cell mass and acceptable trophectoderm grades show higher ongoing pregnancy and live‑birth rates.
Some studies report limited predictive value once euploid, but larger cohorts still find morphology adds useful guidance for selection decisions.
Other factors matter too, like endometrial conditions and patient age, ovarian reserve, and overall reproductive health, so embryo quality helps prediction but does not guarantee success.
These other influences on implantation are worth considering alongside embryo morphology.
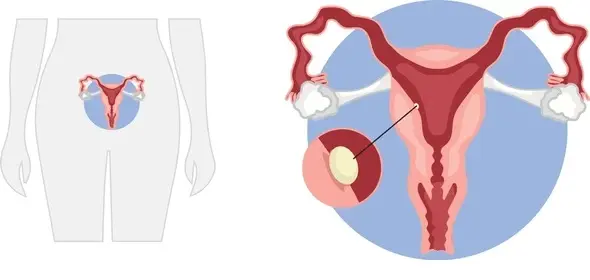
Beyond embryo quality, three pillars drive implantation: endometrial receptivity, embryo transfer technique, and patient factors. Receptivity depends on timing the window of implantation and a healthy lining. Uterine issues like polyps or fibroids can lower success.
Transfer skill and simplicity matter; gentle placement and optimal positioning improve chances without adding trauma. Patient age, BMI, smoking, alcohol, and underlying conditions also influence outcomes.
Supportive lifestyle steps can help overall success. HMG hormone protocols may benefit from luteal support personalization to align endometrium and reduce confounders during transfer planning.
Personalizing luteal support is one of the most discussed strategies to improve outcomes after stimulation.
Personalizing luteal phase support after HMG hormone stimulation can boost implantation by matching care to each patient’s needs and trigger type. Most IVF clinics start progesterone within 1–3 days after egg retrieval. The dose or length may change based on hormone levels and cycle plan.
After an hCG trigger, progesterone alone usually works well. A GnRH‑agonist trigger may need extra support or a small hCG boost in select cases. At Peptide Works, we offer high‑quality HMG and hCG peptides for advanced fertility research to explore the best luteal support strategies.
Looking ahead, ongoing studies are shaping how HMG will be used in future fertility treatment protocols.
The future looks personalized and data-driven. HMG hormone will be paired with smarter monitoring to match dosing, trigger choice, and luteal support to each research protocol. Clinics may blend HMG hormone with targeted LH activity and clear timing rules to improve consistency and reduce risk.
Expect wider use of tailored approaches after retrieval to enhance endometrial readiness and implantation studies.
Peptide Works will continue supporting advanced fertility research with high-quality HMG and hCG peptides, helping scientists test what works best across varied study conditions. This means simpler paths to consistent results, with a focus on safety, access, and real-world data.
All peptides and compounds mentioned are strictly for research purposes only and not for human use.
[1] Gleicher N, Karande V. Generic human menopausal gonadotropin (hMG) in place of more costly follicle-stimulating hormone (FSH) for routine ovulation induction. J Assist Reprod Genet. 2000 Oct;17(9):489-95.
[2] Lou H, Li N, Guan Y, Zhang Y, Hao D, Cui S. Association between morphologic grading and implantation rate of Euploid blastocyst. J Ovarian Res. 2021 Jan 23;14(1):18.
[3] Ghasemian F, Faraji R, Asgharnia M, Zahiri Z, Bahadori MH. The impact of different time intervals between hCG priming and oocyte retrieval on ART outcomes. Iran J Reprod Med. 2013 Jul;11(7):559-64.
[4] Gan R, Huang X, Zhao J, Zhang Q, Huang C, Li Y. Time interval between hCG administration and oocyte retrieval and ART outcomes: an updated systematic review and meta-analysis. Reprod Biol Endocrinol. 2023 Jul 3;21(1):61.
[5] Singh N, Kashyap A, Malhotra N, Mahey R,et al. Comparison of the effects of two different trigger strategies – dual (hCG + Leuprolide) versus hCG trigger – in antagonist non-donor IVF: a randomized controlled trial. JBRA Assist Reprod. 2023 Sep 12;27(3):467-473.
ALL CONTENT AND PRODUCT INFORMATION AVAILABLE ON THIS WEBSITE IS FOR EDUCATIONAL PURPOSES ONLY.
DISCLAIMER: These products are intended solely as a research chemical only. This classification allows for their use only for research development and laboratory studies. The information available on our Peptide Works website: https://peptide-works.com/ is provided for educational purposes only. These products are not for human or animal use or consumption in any manner. Handling of these products should be limited to suitably qualified professionals. They are not to be classified as a drug, food, cosmetic, or medicinal product and must not be mislabelled or used as such.
Peptide Works
Related Articles

What are the Best Cognitive Peptides?
Cognitive peptides are short chains of amino acids that researchers are exploring for their potential effects on brain function. They

Achieving increased skin pigmentation without prolonged sun exposure has been demonstrated with Melanotan peptides in research. Two commonly studied options,

Can PTD-DBM Hair Growth Peptide Stop Balding?
Hair thinning and balding affect millions worldwide, often leading to frustration and limited options. This challenge has driven researchers to