
PROMO!
First order? Get 10% OFF with this code: 1storder
Written by

Bronchogen is a short peptide with the sequence Ala-Glu-Asp-Leu (AEDL) studied for its effects on lung tissue structure and airway function. Research in chronic obstructive pulmonary disease models shows that Bronchogen influences the balance of epithelial cells lining the airways. In these models, peptide treatment normalized cell composition, reduced excessive mucus-producing cells, and restored populations of ciliated cells that clear particles from the lungs. These changes correlate with improved airway barrier function.
Studies also report that Bronchogen reduces local neutrophilic inflammation and shifts pro-inflammatory cytokine profiles in lung fluid toward normal levels. These outcomes matter to COPD research because chronic inflammation and epithelial remodeling drive disease progression. The peptide’s small size and targeted activity make it a subject of interest for continuing lung-focused peptide research.
To appreciate why Bronchogen’s effects draw attention, it is important to understand one of the core challenges that defines COPD at the airway level.
Explore Bronchogen from Peptide Works, a short peptide that supports airway cell balance and epithelial health to aid lung tissue function in COPD research.
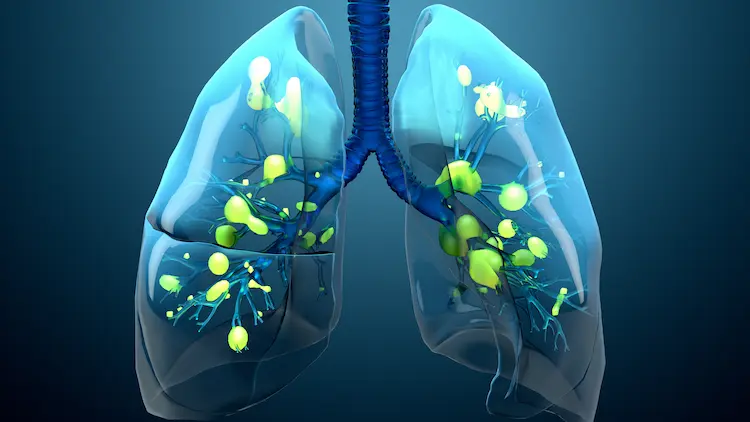
In COPD research, scientists find that mucus overproduction results from changes in airway secretion control. Chronic exposure to smoke and irritants triggers goblet cell hyperplasia, which increases the number of mucus-secreting cells along the airway surface. At the same time, submucosal glands enlarge and release higher levels of mucin proteins such as MUC5AC, making mucus thicker and more abundant. These changes cause mucus to accumulate in the airway lumen and restrict airflow.
Research models that include Bronchogen focus on how lung-targeted peptides behave in airway environments dominated by persistent mucus accumulation. This focus allows researchers to examine peptide behavior under real COPD-like conditions, where mucus overload plays a defining role in airway dysfunction.
Mucus buildup does not remain a static problem. When retention continues over time, it begins to influence how COPD advances and worsens.

Persistent mucus retention in COPD creates a physical and biological environment that drives disease progression. Thick, immobile secretions trap bacteria and other pathogens, increasing the risk of chronic infection and ongoing airway irritation. This environment promotes repeated cycles of acute flare-ups and sustained airway stress, which accelerates overall damage to respiratory tissues.
Reduced mucus transport also contributes to airflow limitation and progressive decline in lung function over time. Studies show that patients with chronic mucus retention experience a faster reduction in measures such as FEV₁ and a higher rate of hospitalizations due to exacerbations.
While Bronchogen addresses specific airway-related pathways, COPD research also considers additional peptides when examining broader respiratory and immune interactions.
COPD research discussions sometimes reference other peptides alongside Bronchogen when examining broader respiratory and immune-related pathways.
These peptides appear in COPD-related literature as part of wider research contexts and are often discussed independently of airway structure, mucus dynamics, or epithelial regulation.
Shop VIP Peptide from Peptide Works, a neuropeptide that helps regulate airway tone and immune signaling for improved respiratory function.

Vasoactive Intestinal Peptide (VIP) is studied in COPD research because it influences both airway smooth muscle function and immune signaling pathways linked to chronic obstructive pulmonary disease. VIP interacts with VPAC1 and VPAC2 receptors that are present in airway smooth muscle and immune cells, and its signaling promotes relaxation of airway muscle and affects pathways that regulate immune balance. Research identifies VIP’s bronchodilatory properties and involvement in airway homeostasis, which are relevant to airflow limitation seen in COPD models.
Studies also examine VIP because its role in immune modulation and airway responsiveness intersects with key features of chronic lung obstruction. Research explores how altered VIP signaling and receptor expression may relate to airway constriction and chronic immune activity in obstructive airway conditions.
Immune imbalance remains a major factor in COPD severity, which directs attention toward another peptide discussed in this research space.
Research on Thymosin Alpha-1 (Tα1) in COPD focuses on its effects on immune function and the inflammatory response in chronic obstructive pulmonary disease. Clinical studies show that adding Thymosin Alpha-1 to standard care in acute exacerbations of COPD can increase CD4+ T lymphocytes, raise the CD4+/CD8+ ratio, and reduce CD8+ counts, indicating enhanced cellular immune activity. Tα1 treatment is also associated with improved pulmonary function measures (FEV1 and FEV1/FVC) and better arterial oxygen levels compared with routine therapy alone.
These immune shifts correspond to decreased inflammatory markers and lower exacerbation frequency in the study groups, suggesting that Thymosin Alpha-1 may support immune regulatory pathways relevant to COPD-related immune dysfunction.
Viewed together, these peptide-focused research areas point toward a broader shift in how COPD is studied at the molecular level.
Checkout Thymosin Alpha-1 from Peptide Works, a peptide that supports immune regulation and helps modulate inflammatory responses in chronic lung conditions.
Research on Bronchogen reflects a broader shift toward targeted peptide approaches in COPD studies. Early findings show that lung-focused peptides can engage specific cellular and signaling pathways involved in airway dysfunction, offering researchers a more precise way to study complex disease mechanisms beyond generalized models.
As COPD research continues to evolve, interest in peptides such as Bronchogen, VIP, and Thymosin Alpha-1 is likely to expand. Ongoing investigation into these peptides may help clarify how molecular-level regulation influences airway behavior, immune balance, and disease progression. This direction supports a hopeful outlook for future COPD research driven by peptide-based strategies.
All products discussed are supplied for research purposes only and are not intended for human use.
[1] Titova ON, Kuzubova NA, Lebedeva ES, Preobrazhenskaya TN, et al. [ANTIINFLAMMATORY AND REGENERATIVE EFFECT OF PEPTIDE THERAPY IN THE MODEL OF OBSTRUCTIVE LUNG PATHOLOGY]. Ross Fiziol Zh Im I M Sechenova. 2017 Feb;103(2):201-8.
[2] Wu D, Lee D, Sung YK. Prospect of vasoactive intestinal peptide therapy for COPD/PAH and asthma: a review. Respir Res. 2011 Apr 11;12(1):45.
[3] Jia Z, Feng Z, Tian R, Wang Q, Wang L. Thymosin α1 plus routine treatment inhibit inflammatory reaction and improve the quality of life in AECOPD patients. Immunopharmacol Immunotoxicol. 2015;37(4):388-92.
ALL CONTENT AND PRODUCT INFORMATION AVAILABLE ON THIS WEBSITE IS FOR EDUCATIONAL PURPOSES ONLY.
DISCLAIMER: These products are intended solely as a research chemical only. This classification allows for their use only for research development and laboratory studies. The information available on our Peptide Works website: https://peptide-works.com/ is provided for educational purposes only. These products are not for human or animal use or consumption in any manner. Handling of these products should be limited to suitably qualified professionals. They are not to be classified as a drug, food, cosmetic, or medicinal product and must not be mislabelled or used as such.
Peptide Works
Related Articles

Cartalax Benefits for Aging: Supporting Joint and Tissue Health Naturally
Aging affects how joints move and how tissues handle daily stress. Over time, movement may feel less smooth, and tissues

Why Is the Cartalax Peptide a Game-Changer for Cartilage Health?
The cartalax peptide stands out in cartilage health research due to its defined tripeptide structure and its use as a

Bronchogen Peptide in Pulmonary Fibrosis Studies
Research on pulmonary fibrosis has expanded as scientists work to understand why damaged lung tissue forms permanent scars. Instead of